I went to medical school in London for a while and truly it was great fun. This was the 1960s–Beatles, Stones, Carnaby Street–and if you were going to be anywhere on the planet, central London was it.
The newly released thriller “Last Night in Soho” really captures the atmosphere. Middlesex, my assigned hospital, was located in the very heart of Soho. It had a pub in the basement where doctors, nurses, students, and even a few patients gravitated around 4 pm. I knew I wasn’t in Kansas anymore.
I finished my London rotation with precisely two pieces of memorable knowledge. First, I was endlessly reminded by fellow students, “We’re not at all like you Americans. Medical students here learn to be gentlemen first, doctors second.” This was usually delivered on a waft of warm beer breath, so I couldn’t take it too seriously, but I liked the line. It went well with the phony British accent I was developing.
Second, and this from a highly respected (and genuine knighted Sir) inebriate physician with a W.C. Fields nose: “Lab tests. You American doctors with your lab tests. If you just listen to your patient long enough and use your brain, you’ll make the diagnosis. Then use the lab test to confirm your diagnosis, not make it. The amateur doctor orders lots of tests and looks for one abnormal result. The expert orders one test to confirm what he already has deduced.”
Believe me, when you’re a 20-something medical student standing in the corridor of a hospital founded in 1745, that sounds like the key to everything.
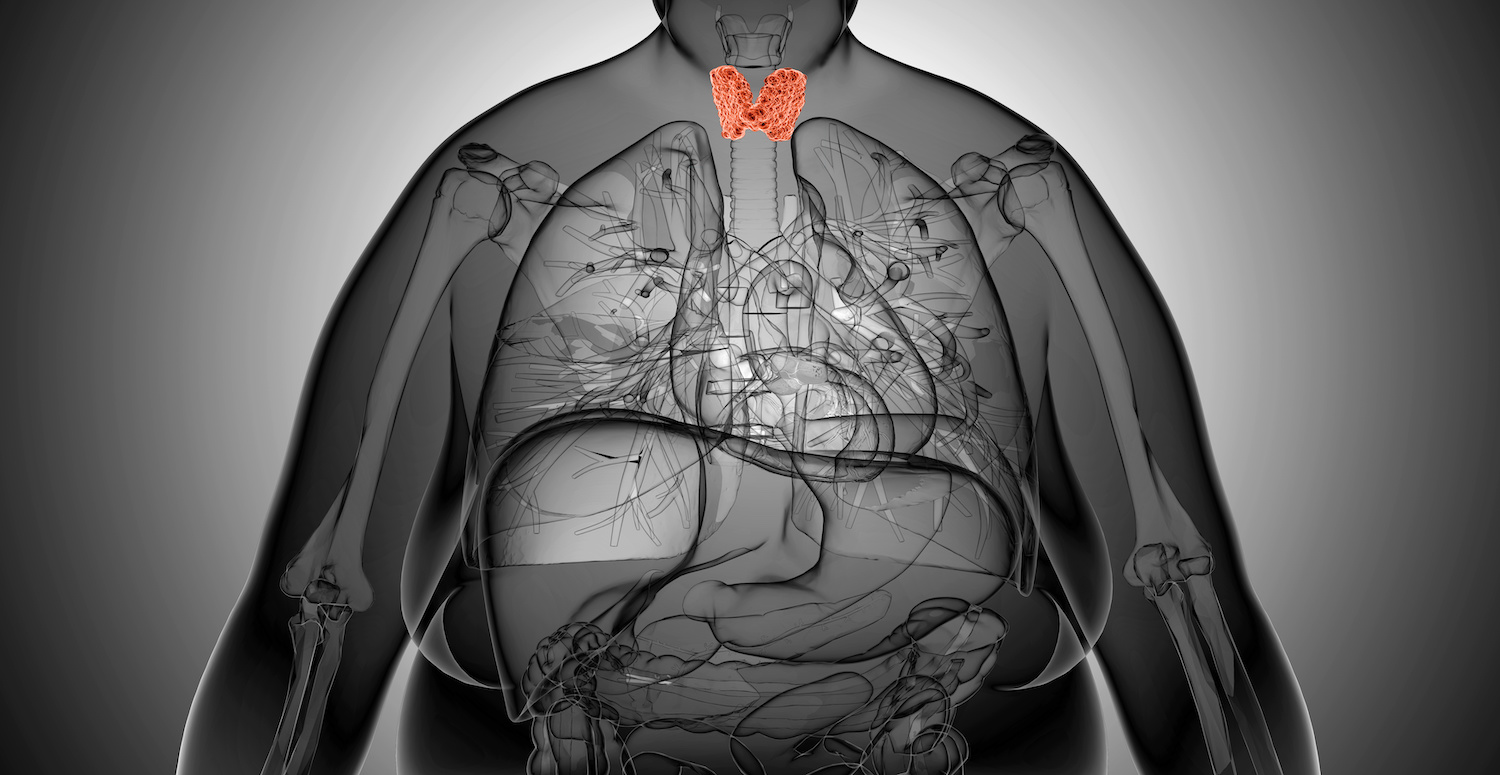
Sadly, the simple rule about listening to the patient and limiting tests never did manage to cross the Atlantic. As a result, millions of women (and many men as well, but women are primarily affected) experience a wide spectrum of underactive thyroid symptoms yet perpetually hear, “I know your symptoms do sound like low thyroid, but see for yourself–your tests are normal.”
Symptoms
The primary low thyroid symptom is feeling tired, a sense of fatigue that usually starts in your 30s and slowly gets worse. You’re not so tired that you’re confined to bed, but you’ve started turning down social invitations, and maybe when you’re with friends in the evening you’re the first to go home because you’re just tired out. You didn’t used to feel this way. You wonder if it’s chronic fatigue syndrome.
You’re also dismayed with your gradual weight gain and inability to lose it. With the dry skin, dry hair, and hair thinning (and thinning of the outer third of your eyebrows), facial puffiness, mental sluggishness, cold hands, cold feet, being always the coldest one in a group of people, and constipation.
Having had low thyroid once myself, I describe it as a strange sense of internal coldness. You’re outside and it’s in the 90s, but you feel cold inside.
You mention this to your doctor during your regular wellness exam or Pap smear and all your tests, including a single thyroid screening test, end up being normal.
Causes
After age 40, it’s estimated about 25% of people have symptoms of diminished thyroid function, called hypothyroidism. There are two causes.
First, a condition called Hashimoto’s thyroiditis, an autoimmune disorder in which the immune system starts creating antibodies against the thyroid gland (and only the thyroid gland), slowly but relentlessly destroying it. Most doctors won’t treat Hashimoto’s until hormone levels fall into the abnormally low range
Second, a controversial condition called thyroid fatigue. In this case, the gland is simply pooped out, exhausted (often along with your adrenal glands) from having received incessant fight-or-flight stress messages along the emergency path from your brain. These messages are relayed via your pituitary, the master gland that controls both thyroid and adrenals.
It’s been the medical profession’s over-reliance on the familiar TSH (thyroid-stimulating hormone) test, developed in the 1960s, that’s led to so much missed hypothyroidism.
(You may need to read these next sentences twice. It confuses medical students, too.) TSH is released by the pituitary, located just beneath your brain, to stimulate your thyroid to make more of its hormone. The pituitary has a hormone-sensing system, so when thyroid hormone levels are low, TSH levels will increase in an effort to boost them.
This is the rule that US doctors are taught: if your patient has a high TSH,
thyroid hormone must be low. Period. The end.
If the TSH test is normal, even though you the patient may have every low-thyroid symptom in the book, your doctor will simply not consider underactive thyroid as a diagnosis. By the way, the opposite is also true. Too much hormone (hyperthyroidism) lowers TSH levels, sometimes as low as zero.
Depending on the lab your doctor uses, the official normal range for TSH is generally between 1.0 and 5.0. If your TSH is above 5.0, you’re declared hypothyroid (you have low thyroid) and you’ll be started on thyroid replacement hormone. To this day, if you go to the doctor with every single symptom of hypothyroidism listed above and your TSH is 4.9, you’ll be told, “Let’s keep an eye on it” and you’ll leave the office untreated, feeling just as crappy as when you arrived.
It’s even worse if your hypothyroidism is due to thyroid fatigue, because in this situation, your pituitary, having been bombarded with stress messages from your brain, is fatigued and depleted as well. So you’ll have all the symptoms of low thyroid and a “mysteriously” low TSH. Your doctor may shake his head in wonderment, “I agree. You sure look hypothyroid, and your hormone levels are on the low side, too, but your TSH is so low, why, you’re almost hyperthyroid.”
You hand him an article from the internet. “Thyroid fatigue? Never heard of it.”
Breakthrough recommendations
Recent research in laboratory testing has uncovered three important breakthroughs that haven’t filtered down to most conventional labs and therefore to most primary care offices.
- The upper limit of normal for TSH should be lowered from 5.0 to 2.5 If this were enacted, the millions of patients with TSH ranges between 2.5 and 5.0 who’d been told they were normal would actually be diagnosed with low thyroid. Most people feel best when their TSH is somewhere between 1.0 and 2.0.
- When hypothyroidism is even remotely suspected the actual levels of hormones themselves (T3 and T4) should be checked. The presence of antibodies against the thyroid gland, which can indicate Hashimoto’s, should also be checked. The presence of these antibodies alone, even with seemingly normal hormone levels, is often enough to warrant starting thyroid replacement therapy. If you have thyroid antibodies, your thyroid function will eventually diminish. Why postpone treatment?
- Since there’s really no lab test for thyroid fatigue, we need to return to an old- fashioned but reliable means of testing thyroid function–measuring basal body temperature. This is your temperature just as you emerge from sleep. Readings of 97.6 degrees or lower were, for your grandmother’s doctor, diagnostic of hypothyroidism, and she’d receive a bottle of natural thyroid from her pharmacist to restore her thyroid hormone levels.
If you want to get started on your thyroid health immediately, order BMR Complex from our Apothecary. It contains all the substances your thyroid needs to manufacture its hormone, but it definitely doesn’t treat hypothyroidism. For that you’ll need actual thyroid hormone. The initials BMR stand for basal metabolic rate, a medical term for the rate at which your body uses energy. If you’re hypothyroid, you have a low BMR.
It’s estimated that tens of millions of people have undiagnosed mild low-thyroid and are chronically fatigued because of it. Tens of thousands of women are undergoing expensive infertility treatments because their fertility specialists are reluctant to prescribe thyroid hormone (even though pregnancy is virtually impossible when your thyroid is underactive).
And all because these physicians weren’t in Professor (Sir) Carrick’s lecture hall that morning as I listened to the elderly bleary-eyed old debauchee raise his finger skyward and ring out with, “Treat the patient, not the lab test!”
It’s a pity we don’t.
Be well,
David Edelberg, MD